Left lying in excrement for 20 hours and scenes ‘like war films’: The elderly patients neglected in NHS hospitals
Elderly patients have been left languishing in their own excrement and puddles of urine for hours on end in NHS hospitals, a major charity has said.
Corridor care is a “crisis in plain sight” in A&Es across the country, charity Age UK warned ministers, as it described “truly shocking” incidents of poor care of elderly people waiting days on end for attention.
In a report, published on Friday, Age UK revealed “heartbreaking” incidents of poor care, including a woman dying from a heart attack after being left to wait; a patient who was “lost” after being put on a disused corridor; and a man left hooked up to an IV drip in a chair for 20 hours, who soiled himself because he was unable to get to the toilet.
People told the charity about “puddles of urine” on the floor as immobile patients are unable to go to the toilet, and patients are being forced to use bedpans in corridors.
Another person said their 86-year-old family member was “stuck in a disused corridor for 36 hours” while “staff kept saying he hasn’t been admitted by the ambulance crew”. A 79-year-old woman from south London told the charity: “The corridors were lined with patients on trolleys, hooked up to drips, some moaning in pain. It reminded me of war films, with queues of stretchers and people suffering.”
Age UK warned that many patients are unwilling to go to A&E, even if they are in a life-threatening situation, because of their past experiences.
It called on the government to “urgently” tackle corridor care as it warned that older people are disproportionately affected.
Caroline Abrahams, charity director of Age UK, said: “What’s happening to some very ill older people when they come to A&E is a crisis hiding in plain sight which the government must face up to and take immediate action to resolve.
“No one should have to spend their final days in a hospital corridor where it’s impossible for the staff to provide good, compassionate care, and it’s truly shocking that this is what is happening to some very old people in some hospitals, today and every day.
“And as we head into winter, we fear that an already very difficult situation in and around some A&Es will get even worse.”
The report comes after The Independent revealed warnings from top medics over a potential “armageddon” facing the NHS this winter, with rising Covid and flu cases alongside staffing cuts.
Health minister Karin Smyth said in response to the Age UK findings: “The stories in this report are heartbreaking. No one should receive care in a corridor – it’s unacceptable, undignified, and we are determined to end it.
“To tackle a problem, you’ve got to be honest about it. For the first time, the NHS will measure and publish the number of patients waiting in corridors. Sunlight is the best disinfectant.”
She said the government is investing £450m to build same-day urgent and emergency care centres, buying 500 new ambulances, and building 40 new mental health crisis centres. She also urged families to get vaccinated.
‘Floods of tears’
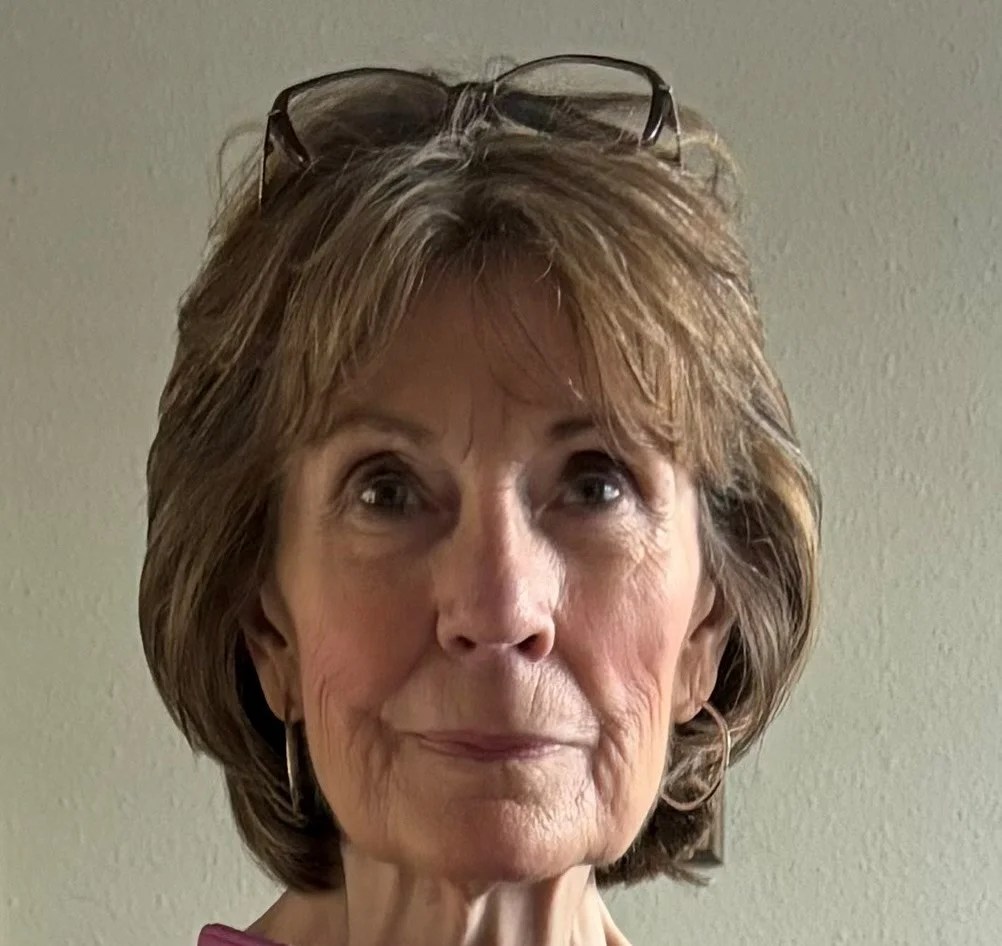
Katherine, a retired NHS nurse from Norfolk, told The Independent how she was left “in floods of tears” after being forced to sit in a chair for hours in pain as she waited in A&E.
Two years ago, Katherine, now 77, underwent surgery for colorectal cancer. Since then, she has faced repeated trips to A&E, often arriving by ambulance due to the severity of her symptoms.
On one occasion, Katherine was admitted to hospital after attending A&E over heart problems, where she was placed on a trolley in the corridor for several hours directly outside the only toilet serving the entire A&E department.
The former nurse described the situation as “an absolute nightmare”, with the smell, the noise of people constantly passing, and staff using a nearby changing area.
During this time, Katherine says she was not offered any food or drink and, eventually, after getting the all clear, was left disoriented trying to find her way out of the hospital on her own.
In another distressing experience, Katherine attended A&E with bowel problems and was left to sit in a chair for hours. She said the lack of privacy and proper facilities left her “in floods of tears”.
“I can feel that things are going to happen, and I’m sitting right next to other people, which is very unpleasant, as you can imagine,” she said.
The former nurse said her A&E experiences have left her frightened of hospital admission after seeing older people sitting on the floor, and on one occasion, a woman bleeding heavily in the waiting room with no one to attend to her.
“Years ago, when you went to the hospital, you felt safe. Now you don’t, you feel absolutely frightened,” she said.
“It was just like a third world country. The basic nursing skills that I remember being taught and would employ seem to have gone out the window. Now it’s all about ticking boxes,” she said, adding that patients are now treated as “figures on a conveyor belt” rather than as human beings.
According to the latest figures for England, some 75 per cent of patients were seen within four hours in A&E in September.
The number of people waiting more than 12 hours in A&E departments in England from a decision to admit to actually being admitted – widely recognised as “corridor care” – stood at 44,765 in September, up from 35,909 in August.
Professor Nicola Ranger, chief executive and general secretary of the Royal College of Nursing, said: “Corridor care is a moral stain on our health service, and this report is yet more evidence of its devastating consequences. No elderly or vulnerable person should be forced to endure these conditions. It is unsafe, undignified, and unacceptable.
“Overstretched and understaffed nursing teams work hard every day to deliver the best care, but they face an impossible task. You simply cannot provide good quality care when patients are lining corridors or are pushed into any other available space.”




